Amputation can be a necessary treatment for trauma, vascular disease, malignant tumors, and other conditions. Amputations occur at different levels and are named accordingly. Those through the tibia bone are referred to as Below Knee (BK) or transtibial, and those through the femur as Above Knee (AK) or transfemoral. In the upper extremity, amputation through the humerus is called transhumeral, or Above Elbow (AE), and those through the forearm bones are Below Elbow (BE). Amputations that occur at the level of the joint are called disarticulations or through joint amputations such as knee disarticulation or through knee amputation (TK). After healing any of these extremity amputations, the residual limb (stump) is fitted for a prosthesis. Traditionally, prosthetic limbs are attached to the residual extremity by being anchored through a socket. The socket is attached to the residual limb through a suction mechanism, straps, or a combination of both.
The component parts of the prosthetic joints, feet, and hands vary by amputation level and are much more sophisticated than they were years ago. However, the connection to the residual limb through a custom molded socket is fundamentally the same for all amputees as it has been for over 100 years. Despite casting or digital scanning in preparation for a perfectly fitted socket, the socket fit remains subject to shrinking and expanding of the residuum from edema or weight loss/gain resulting in the socket being too tight or too loose. In many instances, this, together with the accumulation of moisture from sweating within the socket, is the cause of skin rash, breakdown, and/or infection. These issues can limit prosthetic use time and, in the worst-case scenario, make prosthetic use impossible. In addition, more technologically advanced and computer-assisted prosthetic devices are often too heavy for a socket to stay attached to the upper extremity or short residual lower limb.
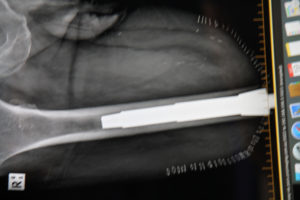
A solution to these socket issues was first developed in 1995 by Dr. Rikard Branemark. It is referred to as ‘osseointegration for amputees’ or OI. OI for amputees relies on the same concepts developed for dental implants, where a metal peg is inserted into the bone of the mandible or maxilla, and a prosthetic tooth is then mounted on this peg. OI for amputees involves the insertion of a metal prosthetic into the central marrow cavity of the bone (medullary canal), with components exiting the skin at the end of the residual limb. The prosthetic limb is then attached directly to the internal metal implant. There is no further need for a socket as the prosthesis now has a direct mechanical attachment to bone. This eliminates the issues related to socket fitting and changes in the contour of the residuum. It also makes donning and doffing (attaching and removing) the prosthesis much easier and faster as it requires a few seconds of simple set screw tightening instead of a typically lengthy process of socket attachment with suction and spacer socks. It also notably allows for heavier prosthetics on the upper extremity as they no longer pull the socket off the arm. This is of critical importance to accommodate more technologically advanced computerized prosthetic arms and hands.
Many of the advantages of an OI attachment over a socket were desired goals from its inception. However, another key advantage called osseoperception was discovered serendipitously. When weight is placed on the prosthetic through an OI implant, it goes directly to the bone, and the vibrations transmitted in this manner allow the patient to feel the ground they are walking on. This phenomenon of being able to sense tapping or touching of the prosthesis itself as well as the underlying ground surface through the connection of the prosthesis is called osseoperception. Osseoperception gives the patient improved balance and responsiveness of the limb during walking on uneven surfaces such as sand, grass, or gravel. It also allows the patient to distinguish surfaces such as tile, carpet, or pavement. Socket prosthetics do not allow for any transmission of information from either the prosthesis or the ground below. Therefore, osseoperception is unique to OI patients, while the socket user relies nearly entirely on visual cues to navigate ambulation.
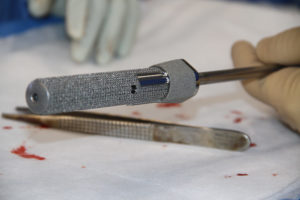
There are currently two major OI implant systems in use around the world with a few others systems being used in relatively small numbers. These systems fall into one of two basic categories in terms of how bony integration is achieved. The first of these is called the OPRA system, Swedish system, or Branemark method. This system relies on a screw-type mechanism and titanium ingrowth surface for bony integration. Using this system, the deep bone implant is inserted at an index surgery, and the soft tissues are closed over it without major revision, and then time is allowed for bony ingrowth. Following bony integration (recommended six months by the company, but can sometimes be shorter), there is a second stage operation where the residual limb is refashioned, and the components that exit the skin are placed within and attached to the now osseointegrated implant.
The other type of system achieves bony integration through a press-fit design similar to what is used for total hip replacement femoral stems. The system that has pioneered and popularized this method and has a very deep clinical experience worldwide is the Osseointegrated Prosthetic Leg (OPL) invented by Dr. Munjed Al Muderis. This system is also known as the Australian system. The OPL is inserted in a single stage where both refashionings of the residuum and implantation occurs at the same time. Bony integration is also achieved through a titanium ingrowth surface, but the method of maintaining stability is through the press-fit of the implant to the bone. In addition to being a single stage, rehabilitation for this type of system is faster with fewer early restrictions.
At present, the use of press-fit systems such as the OPL in the United States is only possible as a custom device for patients not indicated for the OPRA system. For such patients, the implant is designed specifically for their anatomy using modeling from CT images. The Paley Institute is one of only a couple of centers trained in both of these methods and offering both methods of OI as indicated. Given a large number of patients with especially challenging anatomy and clinical history treated at the Paley Institute, this gives us the ability to treat the broadest range of conditions and deep experience with both approaches. The surgery is performed by Drs. Quinnan and Paley at St. Mary’s Medical Center. After a short two-to-three-day hospital stay, patients start rehabilitation under the supervision of Dr. Craig Lichtblau, physiatrist and Director of Rehabilitation for the Paley Institute OI program. Prosthetic fitting is carried out by our Paley Prosthetics prosthetists Matthew Westlake, CO, or Megan Marema, CPO, or in collaboration with your referring prosthetist. Osseointegrated implants can be used with all types of prosthetic components, and newer prosthetics are being designed specially to take full advantage of the OI interface.
Following the operation, the OI connection between the bone and the prosthesis returns the bones to a normal alignment upon standing and walking. This normalizes gait and decreases the energy required for walking. The normalized gait helps protect from arthritis in the other joints and the lower back that results from altered gait. In addition, the natural loading of the hip joint and the femur from the direct mechanical coupling to the bone encourages bone growth. It has been shown to reverse some of the osteoporosis that occurs when ambulating with a socket. Eliminating the bulky socket also provides a much more natural streamlined look in clothes.
OI allows full movement freedom from walking to cycling and recreational activities. Muscular strength is developed freely, minimizing residual limb muscle wasting. Movement of the affected extremity is not restricted by the protruding edges of the socket allowing for greater ease and comfort in sitting, standing, and walking. The direct connection between the femoral bone implant and the knee enables free natural pivoting movements. Patients can also allow the prosthetic connection to rotate, which permits crossing one leg over the other for AK amputees.
Osseointegration can be performed on most skeletally mature extremity amputees. The Paley Orthopedic & Spine Institute is one of less than a handful of centers experienced in using OI technology. The osseointegration procedure and process at the Paley Orthopedic & Spine Institute aims to turn disability into ability, illness to health, and hopelessness to hope. Most indicated patients who receive osseointegration will experience a significant decrease in pain and suffering, an increase in the ability to participate in activities of daily living, and an improvement in quality of life.